What Does Over-Pronation Mean
Overview
One of the most common causes of foot and leg discomfort is a condition known as over pronation. Normal pronation, or "turning inward", of the foot is necessary as the foot adapts to the ground. With over pronation, however, the arch flattens, collapses, and soft tissues stretch. This causes the joint surfaces to function at unnatural angles to each other. When this happens, joints that should be stable now become very loose and flexible. At first, over pronation may cause fatigue. As the problem gets worse, strain on the muscles, tendons, and ligaments of the foot and lower leg can cause permanent problems and deformities.

Causes
There has been some speculation as to whether arch height has an effect on pronation. After conducting a study at the Rose-Hulman Institute of Technology, Maggie Boozer suggests that people with higher arches tend to pronate to a greater degree. However, the generally accepted view by professionals is that the most pronation is present in those with lower arch heights. To complicate matters, one study done by Hylton Menz at the University of Western Sydney-Macarthur suggests that the methods for measuring arch height and determining whether someone is ?flat-footed? or ?high-arched? are unreliable. He says, ?For this reason, studies investigating the relationship between static arch height motion of the rearfoot have consistently found that such a classification system is a poor predictor of dynamic rearfoot function.
Symptoms
When standing, your heels lean inward. When standing, one or both of your knee caps turn inward. Conditions such as a flat feet or bunions may occur. You develop knee pain when you are active or involved in athletics. The knee pain slowly goes away when you rest. You abnormally wear out the soles and heels of your shoes very quickly.
Diagnosis
Pronounced wear on the instep side of shoe heels can indicate overpronation, however it's best to get an accurate assessment. Footbalance retailers offer a free foot analysis to check for overpronation and help you learn more about your feet.

Non Surgical Treatment
Over-Pronation can be treated conservatively (non-surgical treatments) with over-the-counter orthotics. These orthotics should be designed with appropriate arch support and medial rearfoot posting to prevent the over-pronation. Footwear should also be examined to ensure there is a proper fit. Footwear with a firm heel counter is often recommended for extra support and stability. Improperly fitting footwear can lead to additional foot problems.
Surgical Treatment
HyProCure implant. A stent is placed into a naturally occurring space between the ankle bone and the heel bone/midfoot bone. The stent realigns the surfaces of the bones, allowing normal joint function. Generally tolerated in both pediatric and adult patients, with or without adjunct soft tissue procedures. Reported removal rates, published in scientific journals vary from 1%-6%.
Do I Cure Calcaneal Apophysitis In The Home?
Overview
Sever?s disease is a common cause of heel pain in children especially in the young and physically active. Severs disease is a painful bone disorder that results from inflammation (swelling) of the growth plate in the heel. A growth plate, also called an epiphyseal plate, is an area at the end of a developing bone where cartilage cells change over time into bone cells. As this occurs, the growth plates expand and unite. It is very important that damage to the growth plate is avoided.
Causes
Overuse and stress on the heel bone through participation in sports is a major cause of calcaneal apophysitis. The heel?s growth plate is sensitive to repeated running and pounding on hard surfaces, resulting in muscle strain and inflamed tissue. For this reason, children and adolescents involved in soccer, track, or basketball are especially vulnerable. Other potential causes of calcaneal apophysitis include obesity, a tight Achilles tendon, and biomechanical problems such as flatfoot or a high-arched foot.
Symptoms
The main symptom of sever's disease is pain and tenderness at the back of the heel which is made worse with physical activity. Tenderness will be felt especially if you press in or give the back of the heel a squeeze from the sides. There may be a lump over the painful area. Another sign is tight calf muscles resulting with reduced range of motion at the ankle. Pain may go away after a period of rest from sporting activities only to return when the young person goes back to training.
Diagnosis
The doctor may order an x-ray because x-rays can confirm how mature the growth center is and if there are other sources of heel pain, such as a stress fracture or bone cyst. However, x-rays are not necessary to diagnose Sever?s disease, and it is not possible to make the diagnosis based on the x-ray alone.
Non Surgical Treatment
Orthotics or special shoe inserts can also be used to cushion the heel and reduce pain. Physical Therapy. If avoiding physical activities fails to clear up Sever?s disease Genesis Orthopedics & Sports Medicine may proceed with physical therapy. Physical therapy strengthens the muscles and tendons in the heel, releasing pressure and eventually reducing pain.
Adult Aquired Flat Feet Do I Suffer From AAF?
Overview
PTTD is a common condition treated by foot and ankle specialists. Although there is a role for surgical treatment of PTTD, conservative care often can prevent or delay surgical intervention. Decreasing inflammation and stabilizing the affected joints associated with the posterior tibial tendon can decrease pain and increase functional levels. With many different modalities available, aggressive nonoperative methods should be considered in the treatment of PTTD, including early immobilization, the use of long-term bracing, physical therapy, and anti-inflammatory medications. If these methods fail, proper evaluation and work-up for surgical intervention should be employed.

Causes
Overuse of the posterior tibial tendon is often the cause of PTTD. In fact, the symptoms usually occur after activities that involve the tendon, such as running, walking, hiking, or climbing stairs.
Symptoms
Initially, flatfoot deformity may not present with any symptoms. However, overtime as the tendon continues to function in an abnormal position, people with fallen arches will begin to have throbbing or sharp pain along the inside of the arch. Once the tendon and soft tissue around it elongates, there is no strengthening exercises or mechanism to shorten the tendon back to a normal position. Flatfoot can also occur in one or both feet. If the arch starts to slowly collapse in one foot and not the other, posterior tibial dysfunction (PTTD) is the most likely cause. People with flatfoot may only have pain with certain activities such as running or exercise in the early phase of PTTD. Pain may start from the arch and continue towards the inside part of the foot and ankle where the tendon courses from the leg. Redness, swelling and increased warmth may also occur. Later signs of PTTD include pain on the outside of the foot from the arch collapsing and impinging other joints. Arthritic symptoms such as painful, swollen joints in the foot and ankle may occur later as well due to the increased stress on the joints from working in an abnormal position for a long period of time.
Diagnosis
Looking at the patient when they stand will usually demonstrate a flatfoot deformity (marked flattening of the medial longitudinal arch). The front part of the foot (forefoot) is often splayed out to the side. This leads to the presence of a ?too many toes? sign. This sign is present when the toes can be seen from directly behind the patient. The gait is often somewhat flatfooted as the patient has the dysfunctional posterior tibial tendon can no longer stabilize the arch of the foot. The physician?s touch will often demonstrate tenderness and sometimes swelling over the inside of the ankle just below the bony prominence (the medial malleolus). There may also be pain in the outside aspect of the ankle. This pain originates from impingement or compression of two tendons between the outside ankle bone (fibula) and the heel bone (calcaneus) when the patient is standing.
Non surgical Treatment
Orthotic or anklebrace, Over-the-counter or custom shoe inserts to position the foot and relieve pain are the most common non-surgical treatment option. Custom orthotics are often suggested if the shape change of the foot is more severe. An ankle brace (either over-the-counter or custom made) is another option that will help to ease tendon tension and pain. Boot immobilization. A walking boot supports the tendon and allows it to heal. Activity modifications. Depending on what we find, we may recommend limiting high-impact activities, such as running, jumping or court sports, or switching out high-impact activities for low-impact options for a period of time. Ice and anti-inflammatory medications. These may be given as needed to decrease your symptoms.

Surgical Treatment
Although non-surgical treatments can successfully manage the symptoms, they do not correct the underlying problem. It can require a life-long commitment to wearing the brace during periods of increased pain or activity demands. This will lead a majority of patients to choose surgical correction of the deformity, through Reconstructive Surgery. All of the considerations that were extremely important during the evaluation stage become even more important when creating a surgical plan. Generally, a combination of procedures are utilized in the same setting, to allow full correction of the deformity. Many times, this can be performed as a same-day surgery, without need for an overnight hospital stay. However, one or two day hospital admissions can be utilized to help manage the post-operative pain. Although the recovery process can require a significant investment of time, the subsequent decades of improved function and activity level, as well as decreased pain, leads to a substantial return on your investment.
Achilles Tendinitis Treatments And Causes
Overview
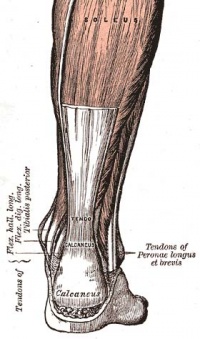
 A tendon is a tough yet flexible band of fibrous tissue. The tendon is the structure in your body that connects your muscles to the bones. The skeletal muscles in your body are responsible for moving your bones, thus enabling you to walk, jump, lift, and move in many ways. When a muscle contracts it pulls on a bone to cause movements. The structure that transmits the force of the muscle contraction to the bone is called a tendon. Tendons come in many shapes and sizes. Some are very small, like the ones that cause movements of your fingers, and some are much larger, such as your Achilles tendon in your heel. When functioning normally, these tendons glide easily and smoothly as the muscle contracts. Sometimes the tendons become inflamed for a variety of reasons, and the action of pulling the muscle becomes irritating. If the normal smooth gliding motion of your tendon is impaired, the tendon will become inflamed and movement will become painful. This is called tendonitis, and literally means inflammation of the tendon.
A tendon is a tough yet flexible band of fibrous tissue. The tendon is the structure in your body that connects your muscles to the bones. The skeletal muscles in your body are responsible for moving your bones, thus enabling you to walk, jump, lift, and move in many ways. When a muscle contracts it pulls on a bone to cause movements. The structure that transmits the force of the muscle contraction to the bone is called a tendon. Tendons come in many shapes and sizes. Some are very small, like the ones that cause movements of your fingers, and some are much larger, such as your Achilles tendon in your heel. When functioning normally, these tendons glide easily and smoothly as the muscle contracts. Sometimes the tendons become inflamed for a variety of reasons, and the action of pulling the muscle becomes irritating. If the normal smooth gliding motion of your tendon is impaired, the tendon will become inflamed and movement will become painful. This is called tendonitis, and literally means inflammation of the tendon.
Causes
The two most common causes of Achilles tendonitis are Lack of flexibility and Overpronation. Other factors associated with Achilles tendonitis are recent changes in footwear, and changes in exercise training schedules. Often long distance runners will have symptoms of Achilles tendonitis after increasing their mileage or increasing the amount of hill training they are doing. As people age, tendons, like other tissues in the body, become less flexible, more rigid, and more susceptible to injury. Therefore, middle-age recreational athletes are most susceptible to Achilles tendonitis.
Symptoms
The Achilles tendon is a strong muscle and is not usually damaged by one specific injury. Tendinitis develops from repetitive stress, sudden increase or intensity of exercise activity, tight calf muscles, or a bone spur that rubs against the tendon. Common signs and symptoms of Achilles Tendinitis include, gradual onset of pain at the back of the ankle which may develop in several days up to several months to become bothersome. Heel pain during physical activities which may diminish after warming up in early stages, or become a constant problem if the problem becomes chronic. Stiffness at the back of the ankle in the morning. During inactivity, pain eases. Swelling or thickening of the Achilles tendon. Painful sensation if the Achilles tendon is palpated. If a pop is heard suddenly, then there is an increased chance that the Achilles tendon has been torn and immediate medical attention is needed.
Diagnosis
If Achilles tendonitis is suspected, avoid any exercise or activity that causes the pain. It is advisable to see a doctor promptly so that an accurate diagnosis can be made and appropriate treatment recommended. The doctor will take a full medical history and will ask about the nature and duration of the symptoms. They will perform a physical examination of the affected area. Ultrasound scanning may be used to assess damage to the tendon or surrounding structures. Occasionally MRI (magnetic resonance imaging) may be recommended. The symptoms of Achilles tendonitis are often similar to symptoms of other conditions such as partial Achilles tendon rupture and heel bursitis. This can make diagnosis difficult and a referral to an orthopaedic specialist may be required in order for an accurate diagnosis to be made.
Nonsurgical Treatment
NSAIDS like ibuprofen are often prescribed to help manage the pain and inflammation. Steroids are often recommended when patients do not respond to NSAID treatment. They are often most effective when injected directly into the inflamed and swollen area. Physiotherapy is a great way to stretch and strengthen the Achilles tendon. A good physical therapist will also teach the patient techniques which give better foot support during exercise (taping, wrapping, etc?). Orthotics, assistive devices and insoles can be used to cushion and cradle the arch of the foot during the healing process. Shock Wave Therapy. This is the newest form of treatment and uses concentrated sound waves to stimulate healing in the affected area. This form of treatment is reserved for heel pain that is unresponsive to other forms of treatment.
Surgical Treatment
If non-surgical treatment fails to cure the condition then surgery can be considered. This is more likely to be the case if the pain has been present for six months or more. The nature of the surgery depends if you have insertional, or non-insertional disease. In non-insertional tendonosis the damaged tendon is thinned and cleaned. The damage is then repaired. If there is extensive damage one of the tendons which moves your big toe (the flexor hallucis longus) may be used to reinforce the damaged Achilles tendon. In insertional tendonosis there is often rubbing of the tendon by a prominent part of the heel bone. This bone is removed. In removing the bone the attachment of the tendon to the bone may be weakened. In these cases the attachment of the tendon to the bone may need to be reinforced with sutures and bone anchors.
Prevention
Although Achilles tendinitis cannot be completely prevented, the risk of developing it can be lowered. Being aware of the possible causes does help, but the risk can be greatly reduced by taking the following precautions. Getting a variety of exercise - alternating between high-impact exercises (e.g. running) and low-impact exercise (e.g. swimming) can help, as it means there are days when the Achilles tendon is under less tension. Limit certain exercises - doing too much hill running, for example, can put excessive strain on the Achilles tendon. Wearing the correct shoes and replacing them when worn - making sure they support the arch and protect the heel will create less tension in the tendon. Using arch supports inside the shoe, if the shoe is in good condition but doesn't provide the required arch support this is a cheaper (and possibly more effective) alternative to replacing the shoe completely. Stretching, doing this before and after exercising helps to keep the Achilles tendon flexible, which means less chance of tendinitis developing. There is no harm in stretching every day (even on days of rest), as this will only further improve flexibility. Gradually increasing the intensity of a workout - Achilles tendinitis can occur when the tendon is suddenly put under too much strain, warming up and increasing the level of activity gradually gives your muscles time to loosen up and puts less pressure on the tendon.
Precisely What Leads To Tendon Pain Of The Achilles ?
Overview
 Achilles tendinitis is a common condition that causes pain along the back of the leg near the heel. The Achilles tendon is the largest tendon in the body. It connects your calf muscles to your heel bone and is used when you walk, run, and jump. Although the Achilles tendon can withstand great stresses from running and jumping, it is also prone to tendinitis, a condition associated with overuse and degeneration. Simply defined, tendinitis is inflammation of a tendon. Inflammation is the body's natural response to injury or disease, and often causes swelling, pain, or irritation. There are two types of Achilles tendinitis, based upon which part of the tendon is inflamed. Noninsertional Achilles tendinitis, Noninsertional Achilles Tendinitis. In noninsertional In both noninsertional and insertional Achilles tendinitis, damaged tendon fibers may also calcify (harden). Tendinitis that affects the insertion of the tendon can occur at any time, even in patients who are not active.
Achilles tendinitis is a common condition that causes pain along the back of the leg near the heel. The Achilles tendon is the largest tendon in the body. It connects your calf muscles to your heel bone and is used when you walk, run, and jump. Although the Achilles tendon can withstand great stresses from running and jumping, it is also prone to tendinitis, a condition associated with overuse and degeneration. Simply defined, tendinitis is inflammation of a tendon. Inflammation is the body's natural response to injury or disease, and often causes swelling, pain, or irritation. There are two types of Achilles tendinitis, based upon which part of the tendon is inflamed. Noninsertional Achilles tendinitis, Noninsertional Achilles Tendinitis. In noninsertional In both noninsertional and insertional Achilles tendinitis, damaged tendon fibers may also calcify (harden). Tendinitis that affects the insertion of the tendon can occur at any time, even in patients who are not active.
Causes
When you place a large amount of stress on your Achilles tendon too quickly, it can become inflamed from tiny tears that occur during the activity. Achilles tendonitis is often a result of overtraining, or doing too much too soon. Excessive hill running can contribute to it. Flattening of the arch of your foot can place you at increased risk of developing Achilles tendonitis because of the extra stress placed on your Achilles tendon when walking or running.
Symptoms
There are several types of Achilles tendinitis symptoms, but all of them are closely related. People who suffer from Achilles tendon pain typically have swelling in the Achilles tendon, and that pain can be chronic as the microscopic tears in the area become more prevalent over time. The most intense pain is typically located just a few centimeters above the area where the tendon meets the heel. This area is called the watershed zone, and the amount of blood moving through it is what gives it the highest potential for injury, especially for athletes. Most of the Achilles tendinitis symptoms in people with the condition will happen immediately after they have been inactive for a fairly significant amount of time. That means that the most pain will generally be felt after sitting or lying down for an extended period, or right after waking up in the morning and getting moving. If you aren?t positive that you are suffering specifically from Achilles tendinitis symptoms, consult a doctor to make sure.
Diagnosis
Confirming Achilles tendonitis may involve imaging tests. X-rays provide images of the bones of the foot and leg. Magnetic resonance imaging (MRI) is useful for detecting ruptures and degeneration of tissue. Ultrasound shows tendon movement, related damage, and inflammation.
Nonsurgical Treatment
NSAIDs help decrease swelling and pain or fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions. Steroid injections. Steroids decrease pain and swelling. After you get this shot, you may feel like your Achilles tendon is healed. Do not return to your regular exercise until your caregiver says it is okay. You could make the tendinitis worse, or even tear the tendon. Surgery. If your tendinitis does not heal with other treatments, you may need surgery. Surgery may be done to repair a tear in the tendon, or to remove parts of the tendon. The most important way to manage Achilles tendinitis is to rest. Rest decreases swelling and keeps your tendinitis from getting worse. You may feel pain when you begin to run or exercise. The pain usually goes away as your muscles warm up, but it may come back. Your caregiver may tell you to stop your usual training or exercise activities. He may give you other exercises to do until your Achilles tendon heals. Ice decreases swelling and pain. Put ice in a plastic bag. Cover it with a towel. Put this on your Achilles tendon for 15 to 20 minutes, 3 to 4 times each day. Do this for 2 to 3 days or until the pain goes away. After 2 or 3 days, you may use heat to decrease pain and stiffness. Use a hot water bottle, heating pad, whirlpool, or warm compress. To make a compress, soak a clean washcloth in warm water. Wring out the extra water and put it on your Achilles tendon 15 to 20 minutes, 3 to 4 times each day. Stretching and making the muscles stronger may help decrease stress on your Achilles tendon. Physical therapists can teach you exercises and treatments to help your tendinitis heal faster. You may need to wear inserts in your shoes. You may need to wrap tape around your heel and back of the leg. You may need to wear a cast, brace, or support boot.

Surgical Treatment
Surgery is considered the last resort. It is only recommended if all other treatment options have failed after at least six months. In this situation, badly damaged portions of the tendon may be removed. If the tendon has ruptured, surgery is necessary to re-attach the tendon. Rehabilitation, including stretching and strength exercises, is started soon after the surgery. In most cases, normal activities can be resumed after about 10 weeks. Return to competitive sport for some people may be delayed for about three to six months.
Prevention
By properly training the body, an athlete can build the strength of their tendons and muscles. Following a workout and dieting plan, the body will be able to build muscle and strengthen most effectively. Additionally, doing the following can prevent tendinitis. Wearing appropriate shoes will give your foot the support it needs for proper movements of the foot and ankle. Improper movements will put additional stress on your body. Stretching before an athletic activity, Stretching primes the body for a taxing activity. Additionally, this will get your blood flowing and reduce the risk of pulling a muscle. Ask your doctor about orthotics, Custom orthotics can help get your foot into proper alignment. If the foot does not execute proper mechanics, the body will adjust which will cause pain and increase the chances of injury.
Ruptured Achilles Tendon The Facts
Overview

The Achilles tendon attaches the calf muscles in the leg to the heel bone. It is the largest yet most exposed tendon in the body. An Achilles tendon rupture injury is when the tendon fibres tear, causing symptoms of pain and loss of function. A rupture can be either partial or complete and treatment may involve surgery. Achilles tendon rupture is most common in weekend athletes trying to train too hard and is least common in well-trained professional athletes. The injury is more common in men than in women and the frequency of rupture increases over the age of 30 years.
Causes
Achilles tendon ruptures are most likely to occur in sports requiring sudden stretching, such as sprinting and racquet sports. Achilles tendon ruptures can happen to anyone, but are most likely to occur to middle age athletes who have not been training or who have been doing relatively little training. Common sporting activities related to Achilles tendon rupture include, badminton, tennis, squash. Less common sporting activities that can lead to Achilles tendon rupture include: TKD, soccer etc. Occasionally the sufferer may have a history of having had pain in the Achilles tendon in the past and was treated with steroid injection to around the tendon by a doctor. This can lead to weakening of the tendon predisposing it to complete rupture. Certain antibiotics taken by mouth or by intravenous route can weaken the Achilles tendon predisposing it to rupture. An example would be the quinolone group of antibiotics. An common example is Ciprofloxacin (or Ciprobay).
Symptoms
You may notice the symptoms come on suddenly during a sporting activity or injury. You might hear a snap or feel a sudden sharp pain when the tendon is torn. The sharp pain usually settles quickly, although there may be some aching at the back of the lower leg. After the injury, the usual symptoms are a flat-footed type of walk. You can walk and bear weight, but cannot push off the ground properly on the side where the tendon is ruptured. Inability to stand on tiptoe. If the tendon is completely torn, you may feel a gap just above the back of the heel. However, if there is bruising then the swelling may disguise the gap. If you suspect an Achilles tendon rupture, it is best to see a doctor urgently, because the tendon heals better if treated sooner rather than later. A person with a ruptured Achilles tendon may experience one or more of the following. Sudden pain (which feels like a kick or a stab) in the back of the ankle or calf, often subsiding into a dull ache. A popping or snapping sensation. Swelling on the back of the leg between the heel and the calf. Difficulty walking (especially upstairs or uphill) and difficulty rising up on the toes.
Diagnosis
During the clinical examination, the patient will have significantly reduced ankle plantar flexion strength on the involved side. When the tendon is palpated with one finger on either side, the tendon can be followed from the calcaneus to where it "disappears" in the area of the rupture and to where it then returns 2 to 3 cm proximal to the rupture. If the injury is recent, the patient indicates that her pain is localized at the site of the rupture. The defect eventually fills with blood and edema and the skin over the area becomes ecchymotic.
Non Surgical Treatment
Non-surgical treatment of Achilles tendon rupture is usually reserved for patients who are relatively sedentary or may be at higher risk for complications with surgical intervention (due to other associated medical problems). This involves a period of immobilization, followed by range of motion and strengthening exercises; unfortunately, it is associated with a higher risk of re-rupture of the tendon, and possibly a less optimal functional outcome.

Surgical Treatment
This condition should be diagnosed and treated as soon as possible, because prompt treatment probably improves recovery. You may need to be referred urgently to see a doctor in an orthopaedic department or accident and emergency department. Meanwhile, if a ruptured Achilles tendon is suspected, you should not put any weight on that foot, so do not walk on it at all. A new piece of research found that surgery and conservative treatment actually gave equally good results, when patients were also given early mobilisation treatment using a brace. If an operation is needed, there is a type of surgery called percutaneous, which uses smaller cuts than the traditional operation. This seems to reduce the risk of getting a wound infection. After surgery, a brace seems to be better than a plaster cast in terms of faster recovery and return to normal activities, a lower complication rate and patient preferences.
Prevention
To help reduce your chance of getting Achilles tendon rupture, take the following steps. Do warm-up exercises before an activity and cool down exercises after an activity. Wear proper footwear. Maintain a healthy weight. Rest if you feel pain during an activity. Change your routine. Switch between high-impact activities and low-impact activities. Strengthen your calf muscle with exercises.